Hospitals face many challenges when capturing project costs—not the least of which includes disparate systems and processes that often result in incomplete and inaccurate information. Cost pressures and the need to validate all investments have brought increased attention to all “projects” of strategic importance to hospitals. Hospital project management goals now include the need to reduce costs, improve quality, and boost the quality of patient care and outcomes. Thus, hospitals must implement effective cost-capture processes. To do so, it helps to examine the barriers to effective project costing to create a better model and gain more confidence in the reported “true costs” of a project.
Challenges
As hospitals seek consistent, reliable data for project costing, here are some of the barriers they must overcome.
Costing Method
Project costing has multiple computational “methods” just like cost accounting, which has evolved from cost supply and labor to time-driven cost accounting. As both product and service lines continue to evolve within the outcome-based healthcare model, health services project costing is more dependent on source expenditure data (the types of cost data available). Meanwhile, finance operations remain challenged by the costing methodology that is chosen for costing and the business definition of the data collected (understanding that the data collected and used may have been collected for other purposes).
Integration
Once a costing method is defined, the data sources must now be re-examined to fully understand how data has been captured (from both internal and external health applications) and then transferred into a project costing model. The required data/information can be resident in financial systems, enterprise budgeting applications, business and clinical supply chain solutions, asset management applications, and staffing systems. As you can see, source data often resides in disparate systems that can lack sufficient integration models to support an efficient and accurate compilation and extraction of data required for project costing.
Inconsistent Departmental Financial Reporting Practices
In general, most hospitals set up project reporting as defined in legacy or clinical cost accounting tools. However, most healthcare business line owners now desire the integration of project costing into their departmental profit and loss statements. In these cases, the departmental profit and loss reports now must include accruals so business line owners can distinguish project expenses from operational expenses. Although many hospitals do not record accruals to avoid overstating outstanding obligations through commitment (future expenditure) accounting, both IT and finance departments struggle with both appropriate allocations and confidence in the projected cost. Capturing all costs is crucial for considerations and a cost accounting primer. Unfortunately, there are many sources of “costs” that may be missed not only due to the complexities of gathering the required data from disparate sources and from inconsistent accounting in department profit and loss statements, but also due to poor data governance that does not enforce hospital-wide data definitions that would allow for solid cost comparisons.
Data Sourcing
Typical hospital costing data elements are found in the various source financial transactions. These must be exported into a project costing model that often is configured for fairly high-level aggregations of hospital spend data. Figure 1 is a typical healthcare data model designed for after “the fact”—meaning the data collected is uniquely defined for each of the various applications. Mapped data has inherent complexities and integration challenges.
Figure 1: Sample Healthcare Data Model

Solution
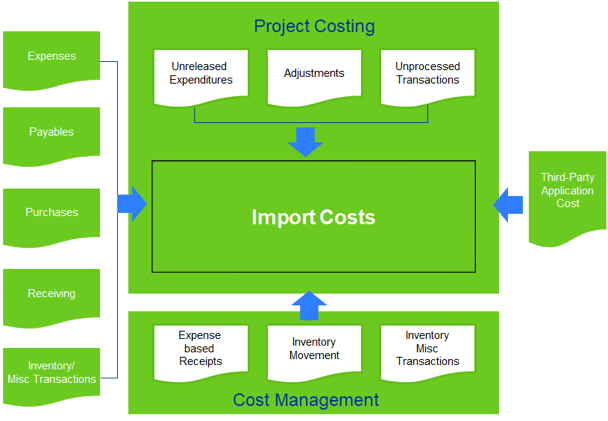
Hospitals can benefit from the development of a project costing integration model based on revised back-office business cloud applications and current clinical systems delivered with artificial intelligence and machine learning tools. These tools deliver a data model similar to the project costing integration model below in Figure 2.
Sierra-Cedar, Inc. now assists healthcare clients in overcoming project costing challenges through the implementation of this project costing integration model, often leveraging the migration from legacy enterprise resource planning (ERP) applications to the vendor’s cloud solution and through the hospital’s implementation of the required data governance models of the clinical systems. For organizations that have chosen not to migrate to a new system, we have redefined data definitions in their current applications. Lessons learned from the implementation of these project costing models facilitate our clients’ ability to obtain a complete set of cost data–including information resident in ERP applications and other back-office financial solutions as well as third-party applications–to enable an accurate and complete project costing process.
Figure 2: Project Costing Integration Model
Once the model is developed, it considers the level of detail for each project’s activity. These levels, supported by drill-down functionality, include a listing of activities the business owners need to manage their service and product line profitably. When it is time to close the project, all the costs are assigned to the project/activity to create the correct balances. It is important that managers respo
nsible for the correct cost coding do this at the beginning of the process to reduce the number of reclassifications and reallocations required. Some other best practices that we deploy when creating a project costing model include:
- Model it on paper first: We evaluate how the hospital’s business owners will use the cost component before bringing them together
- Take advantage of your costing solution’s flexibility: Different solution rules can be used for each area of the business—we leverage that flexibility to optimize results
- Frequent cost collection: Our approach executes data collection frequently to provide ongoing project costing performance throughout the reporting period
- Project set-up features: We maximize feature and function utilization to enhance available reporting information
- Project resource assignment: Our process considers all appropriate labor costs for each project
- Role-Based model access: As projects evolve, access needs change. Our approach provides for governance and access as needed for each project
Summary
As national healthcare reform continues, healthcare entities need to proactively seek both cost savings and effective use of data for better healthcare management. Project costing continues to evolve as the industry embraces news tools and costing methodologies, including cost accounting, to understand product and service line profitability better. Solid data governance is a good start to a sound data model as business owners often define and interpret source data from their business line’s perspective. Sierra-Cedar’s approach begins with a thorough assessment and validation of the project costing element requirements. This philosophy is based on the premise that a project’s true cost cannot be fully understood until a thorough understanding of the functional requirements is obtained. In addition to understanding requirements, the project team and the business owners must establish a consensus understanding of deliverables, assumptions, and the current environment. This must be completed before estimating the time and cost of a project.
Improve Project Costing at Your Organization
Having the right project costing method makes sense for healthcare organizations as fiscal responsibility becomes even more critical to success. Let’s talk more about establishing one for your organization.
